I just discovered this app from the Society of Interventional Radiology (SIR) (Apple App Store | Google Play) that covers all of their guidelines on periprocedural cutoffs and contraindications, such as managing anticoagulation, cutoffs for platelets/INR/etc. Very helpful for referencing if you find yourself frequently consulting IR for things. And free!
Author: Bryan Boling
A Structured Diagnostic Approach for Patients with ARDS
Thanks to Eddy Joe, MD for this article from the journal Critical Care. ARDS is a common problem encountered in ICUs and it can actually result from a number of causes. This paper (HTML | PDF) from Bos and colleagues simplifies things with a diagnostic algorithm (below).
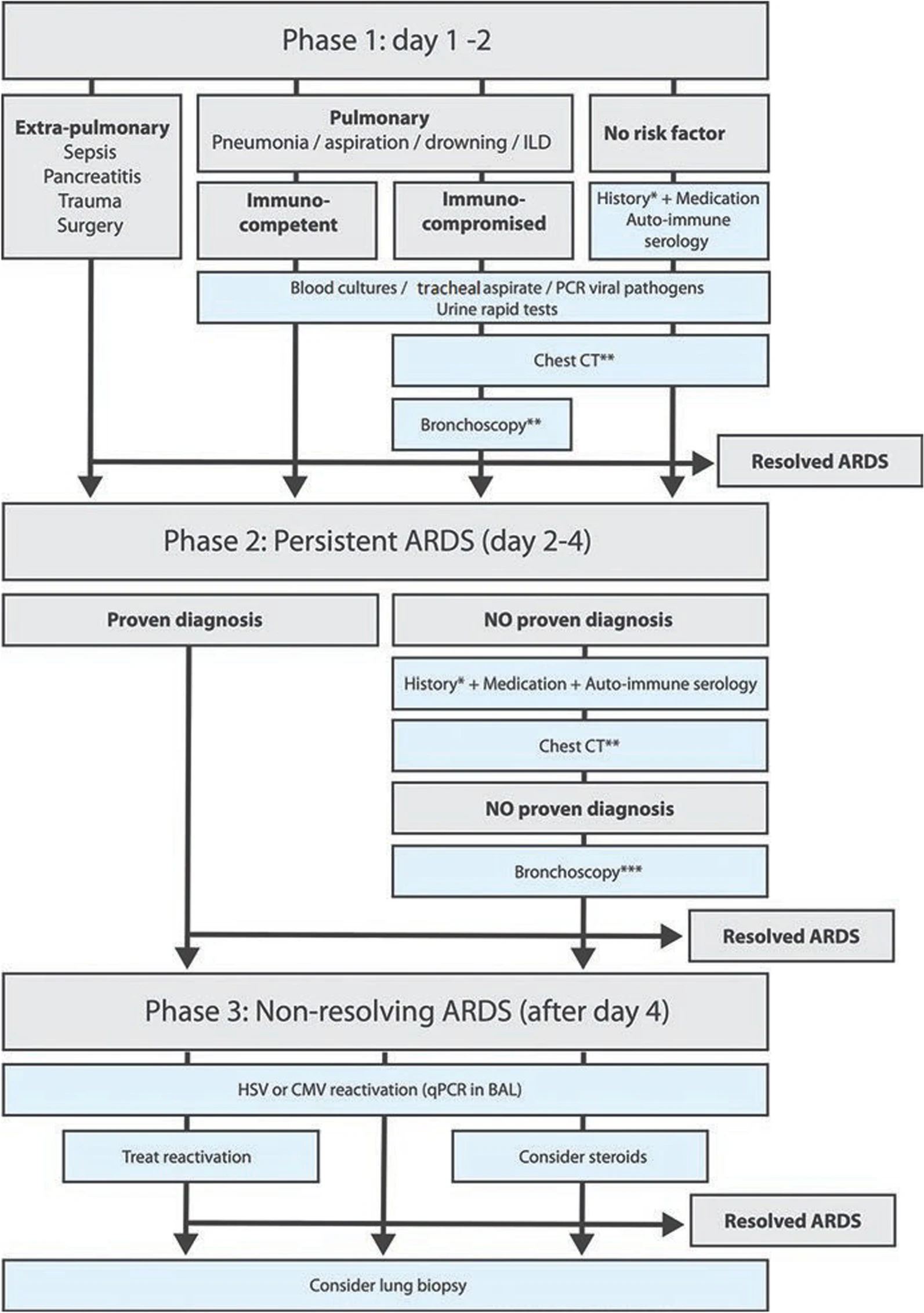
Bos LDJ, de Grooth HJ, Tuinman PR. A structured diagnostic algorithm for patients with ARDS. Crit Care. 2023 Mar 21;27(1):94. doi: 10.1186/s13054-023-04368-y. PMID: 36941668; PMCID: PMC10027589.
Interpreting Clinical Trials
Reading and evaluating clinical trials is one of the tougher things to do as a trainee or new provider. Many times, you only get the minimal amount of training in school and often you don’t pay close enough attention anyway. I find that a lot of trainees think, “I’m here to learn clinical medicine, I’m not interested in research.” But then later realize (hopefully) the benefit of being able to critically read the literature. The extreme responses that I see from a lot of newer providers are, 1) accept everything because it was published in a “good” journal, or because I’ve heard people talking about it on social media/podcast/etc. or 2) give up and just do whatever you see others doing because interpreting it for yourself is too confusing.
So, this quick algorithm from CHEST Critical Care is super helpful. HT to Chris Carroll (@chriscarrollmd.bsky.social). The first image is the pathway that you can follow to ask yourself a few simple questions to decide if this study works for you. That is the key part of this, a study can be “good” and accepted for publication (even in a so-called “good” journal) and still not be something you should implement. The second image just goes over some relevant terms when it comes to research.
Here’s a link to the original article.
Why does myocardial infarction cause ST elevation?
We all know that the ST segment on the ECG elevates when there is myocardial infarction and depresses in the face of myocardial ischemia. But why? I’m a big physiology nerd so it surprised me that I not only didn’t know the answer, but hadn’t even asked the question. I like to understand the why of things to help me remember the what. I can explain why the QRS complex is wide in a bundle branch block (and why you get the “rabbit ears” specifically in a RBBB). Why p waves are bigger in atrial enlargement and why the PR interval is long in AV blocks and short in WPW. So, when I was recently explaining 12-lead ECG interpretation to a group of students, I found myself stumped when I wanted to explain the pathophysiology behind the variations in the ST segment during myocardial ischemia and infarction.
So, I turned to Google and found this article from the Curious Clinicians, a medical podcast that I’ve listened to before (but not this particular episode, apparently) where they discuss the whys of ST elevation and depression. And it turns out, it’s even stranger than I thought…
ECG Interpretation
One of the most common things I’m asked about from new providers is for a good resource to learn 12-lead ECG interpretation. 32bravo711 has a couple of really nice series on YouTube that cover rhythm strip analysis and 12-lead ECG interpretation. It starts with the basics and explains things pretty simply without sacrificing quality.
Brain MRI
This is a subject that I get asked about a lot by students. MRIs are tougher that CTs to read and yet can offer a lot of diagnostic assistance. I’ll be honest, 99% of the time, I rely on the neurologists or neuroradiologists to read these studies. That works for me because, honestly, we never really get these studies stat at our place. So, almost never is an MRI so important that I have to know right away what it shows. But, I’ve become convinced that that is a sort of lazy attitude. And so, I’m making an effort to learn how to better read Brain MRIs. So, you’re in luck, because as I learn, I’m going to pass that on to you. For now, what I’m passing on are a bunch of good resources.
Radiopaedia is ALWAYS a good place to start when looking for all things radiology. They have a really nice Brain MRI course that was a live event a few years back. You can register for the course still and watch the recordings, but there is a cost. For most of us who just want the basics, there is a pre-course video on YouTube that serves as a nice intro.
Rutgers neurology has another really nice video as well. This Brain Imaging Crash Course covers more than just MRI, they address MRI as well as head CT in a nice case-based format (you know I love case-based learning). It doesn’t go terribly in depth, but I suppose that’s why it’s called a crash course instead of “Everything You Need to Know About Brain Imaging.” Another good starter.
If the written word is more your speed, here are two great resources. The first is an excellent Tweetorial introduction to Brain MRI from Lee Alhilali, MD.
There you have a few basic intro resources for reading brain MRIs. Some of you will no doubt want to go deeper, but this is a great starting place. For me, this is what I need to know right now. I’ll let you know if I decide to delve more into all the depths of MRI.
Coronary Artery Dominance
Knowing which coronary artery has the blockage can help you understand the effects of an MI on the myocardium. And seeing regional wall motion abnormalities on echo can often tell you which coronary artery has the blockage. Because certain areas of the heart are supplied by certain coronary arteries. But, there is a trick. In most people, the inferior wall of the heart is supplied by the right coronary artery (RCA), but in some people, it is supplied by the circumflex (LCx). This is known as coronary artery dominance and this Instagram post from our friends over at foamfrat explains it in a little more detail.
Viral Serologies
Viral serologies can be really confusing. But, these make really good boards questions for those of us in acute care medicine. In this Twitter post, @POCUSmedicine shares a really nice infographic about Hepatitis B serologies. While the top left corner is specific to HBV, the general pattern of interpreting serology results is true of all viral serologies. I learned a mnemonic to help remember this when I was studying for boards…IgM = iMMediate, as in active infection is present; IgG = Gone, as in previous exposure.
Airway Notes: The Laryngoscope
In this week’s installment of Airway Notes, we take a look at the laryngoscope used for direct laryngoscopy (DL). DL is becoming a less commonly used skill in favor of video laryngoscopy (VL), but I think it is still an essential skill for airway management. There are 2 main types of blades, the Miller and the MacIntosh and each has its benefits and proponents (I’m a Mac guy, myself). You should be familiar with the use of both, but focus on mastering one before moving on the other.
In the IG post, I show examples of a slightly different way to hold the laryngoscope than how most of us were probably taught. This was taught to me by one of my attendings, an anesthesia critical care physician named Habib Srour. Habib is an incredibly smart guy and when he showed me this technique it instantly made so much sense. It takes the pressure off of the hand and wrist and allows the hand and lower arm to serve as one unit. The force of lifting then is transferred to the elbow and ultimately to the shoulder and upper arm, MUCH stronger than the wrist and forearm. This allows for more lifting force without the urge to rock backwards on the handle, risking damage to the teeth and lips. It is probably the single best tip I’ve gotten in regards to DL.
NG Tube Placement
The nasogastric tube, or NG tube, is one of the most commonly used devices in the ICU. It can be used for removing things from the stomach or adding them (in the form of medication and tube feeding). Although the small bore feeding tube (AKA Dobhoff tube) is becoming the go-to for feeding and oral med administration, even in the short term, the NG tube isn’t going anywhere. This tube is, as its name suggests, inserted into the nare and threaded down the posterior oropharynx and into the stomach. Once it is placed, you need to be sure that it’s placed correctly (you’d be amazed at the places one of these can go!)
This can often be accomplished without the use of radiography, but there are times when an X-ray is needed. The Radiologist covers when and how to use X-ray in the placement of NG tubes.
